The following was written in November of 2020, right after I had taken my final dose of a serotonin reuptake inhibitor drug. While I have since had many insights and revelations, I am sharing this as I wrote it back then. It is a snapshot of a moment in time, and a document of my own process. It is still the most complete single account of my whole drug and withdrawal experience, and what surrounded it. If you are interested in reading something informed by everything I have learned since then, click here.

After nearly 2 decades of Selective Serotonin Reuptake Inhibitor–SSRI–use and 5.5 years of tapering, I took my final dose of Celexa on 11/12/20. So begins the rest of my life.
The following is my story onto and off of antidepressant drugs and what I have learned along the way. Please take from it what resonates with you and leave the rest.
I first started taking Prozac 20mg when I was 15, and I took that final Celexa dose just a month shy of my 34th birthday. As a teenager my home life was difficult, my school life was difficult, my social life was difficult, I was really struggling, therapy wasn’t helping enough, and I felt like I had to do something. I now know that I was dealing with unrecognized complex trauma that manifested as anxiety, depression, and obsessive-compulsive kinds of thought and behavior patterns, but at the time the feedback I kept getting from the people closest to me was that my distress was out of proportion to my life circumstances. So I started taking Prozac. Nobody made me, it was my decision. I could not tolerate things as they were, I believed that there was something wrong with me, and I thought I was being responsible. I was utterly unaware of what a huge impact my environment and the larger culture that surrounded me were having on my mental health and well being (or lack thereof).
I took the Prozac for a couple of years and then stopped “cold turkey” (CT) without tapering because I didn’t like the way it made me feel and I wasn’t convinced it was helping all that much. Sure it kinda took the edge off, but I wasn’t exactly happy. And it made me feel tired all the time and just… not quite like myself. At the time I didn’t notice any issues as a result of my CT stop, although looking back I know now I at least had some brain zaps, if nothing else. When I was 19 and getting ready to start college I was having really bad anxiety and decided to go back on Prozac, but this time around I experienced more notable side effects that I couldn’t deal with. I tried Zoloft briefly and felt terrible on it; I may have tried another med too (I can’t remember now) before I landed on 10mg of Lexapro.
I took 10mg of Lexapro for a couple of years and then in my early 20s my psychiatrist switched me to 20mg of Celexa, saying it was the same thing but less expensive. (Note, it’s not actually the same thing. Lexapro and Celexa are very similar drugs but they are not the same). I don’t remember if I had any side effects from the straight switch or not. I probably did, but I was also living in an incredibly volatile situation and most likely chalked anything odd up to that. A year or so later my dose was upped to 40mg, as I was struggling to deal with atrocious life circumstances that would have probably made even the most well-adjusted person miserable.
When I was 23, I decided it would be a good idea to stop the Celexa CT in the midst of major life changes (not my finest decision making at work there) and made it about 4 months before going back on. I didn’t think about withdrawal at the time, I just assumed my problems–and the onset of panic attacks for the first time–were because my life and my circumstances were so chaotic and because I had something “broken in my brain.” At this point, I also tried adding Wellbutrin but like the Zoloft years before, I didn’t respond well and didn’t stay on it very long, a few weeks maybe.
Are you seeing a theme here yet? An adolescent and young adult with unrecognized trauma and lacking in external support and healthy coping skills to deal with objectively trying life circumstances, understandably feels like she is drowning. This is the literal antithesis of a biological malfunction.
So here I am chugging along through my life on Celexa 40mg, when at the age of 26 there was an issue with my insurance coverage and I was unable to get my drug for about a week. I absolutely lost it. This was not like the other times I had stopped. I could not regulate myself or my emotions at all. Suddenly I was over-the-top irritable, edgy, tearful, angry, agitated, etc. And it really scared me. I knew that prescribers and drug commercials alike always said not to stop antidepressants without talking to the doctor first, but nobody ever told me I would completely derail if I didn’t have it for a few days. And besides, I had just stopped before. But by this point in my life I was already having more and more frequent questions about who I was without the drug, as I had been on one or another of them for so long and since I was so young. After that experience of running out and freaking out, I began to really think about how I could stop for good. When I was 27 I got myself back into therapy after almost a decade away, and when I was 28 I felt ready to begin to taper. This was in the spring of 2015.
The first two years of tapering were really rough because I had no clue what I was doing. I knew I wanted to take it slower than my doctor at the time suggested (he suggested that I cut my dose in half every week or two for a couple of months until I was off; no big deal), but I didn’t consider cuts smaller than 50%. I went from 40mg to 20mg–hard but tolerable after the first few weeks–and held for several months. I went from 20mg to 10mg–much harder but still somewhat manageable after the first month or so–and held for several more months. Then I tried to go from 10mg to 5mg and I stayed there for 4 hellish months hoping to stabilize before deciding to updose back to 10mg. I stayed at 10mg for the better part of a year. During that time I may have even gone back to 20mg for awhile when my job was especially stressful, but I can’t remember now. You get the idea though, it was a lot of large cuts and up-and-down dosing which I now know is the worst way to approach an (S)SRI taper.
In early 2017 I was on 10mg and feeling relatively okay, I thought, and at the advice of a new psychiatrist I decided to try to reduce to 5mg again. He said I could do this for 5 days and then stop. It was only a couple of days into that reduction, in my sleepless agitated desperation, that I found a Facebook group called “SSRIs/Antidepressants Withdrawal (Paroxetine, Paxil, Seroxat).” I wasn’t taking Paxil, but I figured maybe they could help me anyway. And indeed, with my very first post, I went from being afraid I might be stuck on Celexa forever to knowing that there was hope of stopping for good. It was in this group that I learned about the 5-10% taper method, which is backed by peer-reviewed published scientific evidence. (For those who may be unfamiliar, the 5-10% taper method involves reducing your dose by 5-10% or less of your previous dose and holding for several weeks or months before reducing again). From there I got a prescription for liquid Celexa from my internist, updosed again to 8 or 9mg, and began to taper safely. In many ways the tapering got easier over time for me. By the time I found the group I think my central nervous system was so sensitized and dysregulated from the previous 2 years that I spent most of the final 3.5 years of safe tapering trying to heal from the damage I had unwittingly done to myself by attempting to follow various doctor’s medical advice. The more I healed (however slowly), the easier tapering became. I also did nothing but slow down my taper as the years have worn on: when I first found the group I was reducing by 10%, then I started reducing by 5%, and for the last 2 years 1-2%, as I could tolerate less and less the lower my dose dropped. My final dose was 0.04mg.
In terms of all the various withdrawal symptoms I have had over the years there are too many to count, but the most debilitating, pervasive, and unrelenting ones have been extreme fatigue, widespread weakness and pain (that didn’t respond to OTC pain meds), flu-like symptoms, digestive issues/IBS, food/chemical/photo/noise/heat and other environmental sensitivities, exercise intolerance, word recall and memory problems, and chronic itching/burning skin, dermatographia, and seemingly random frequent hives. There were times when I couldn’t really work much, when I couldn’t drive safely, and when I even struggled to form coherent sentences. My quality of life has been impacted profoundly. Happily, today I am doing a whole lot better than I was. Even the worst of the symptoms listed above have improved by about 60-70% overall I’d say with the exception of the skin/allergy related ones. However, I still do not consider myself “fully recovered.” I still have a lot of healing to do.
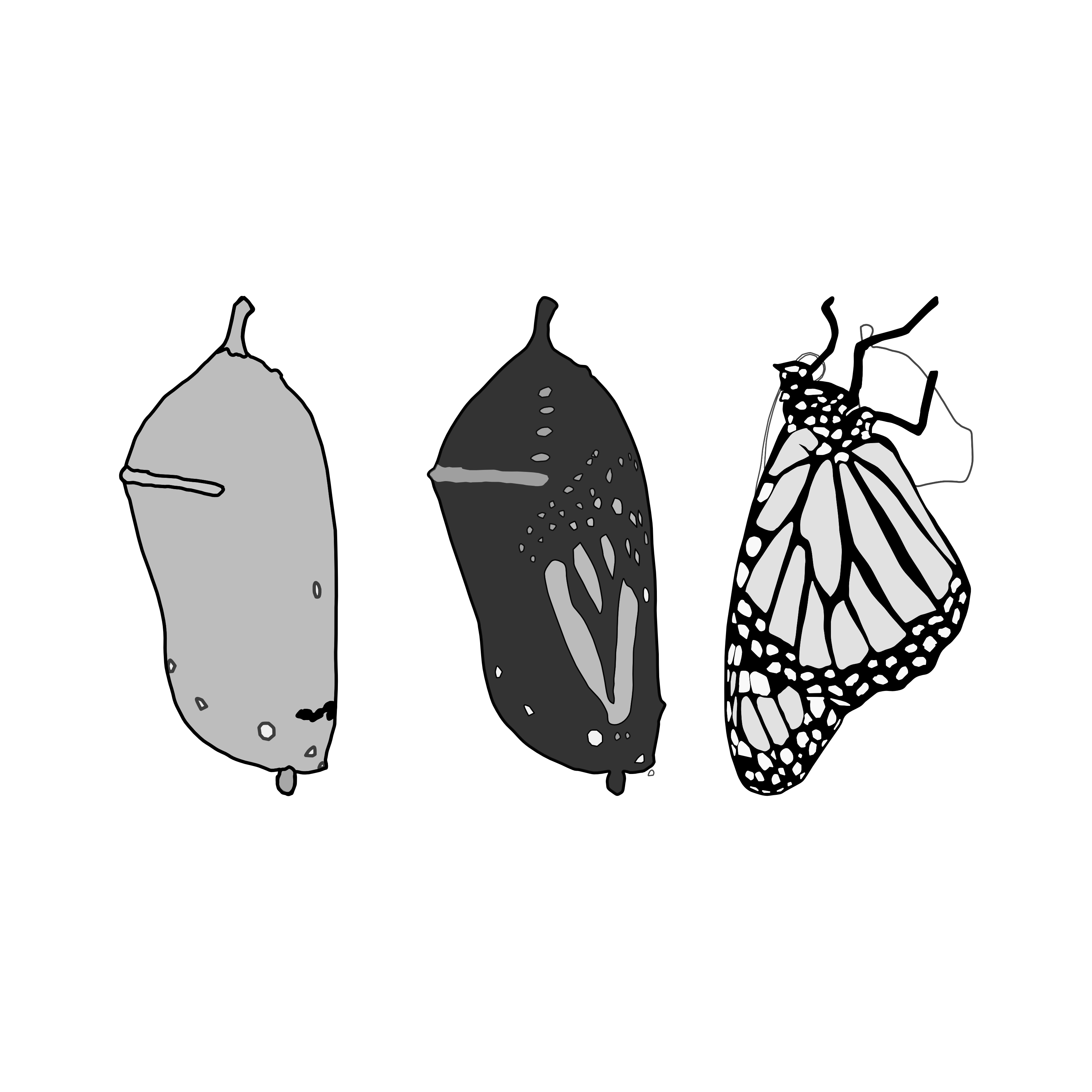
What’s more, I am expecting another few years before I have any idea what my actual baseline is. That’s okay; this journey is not for the faint of heart. It is the hardest thing I have ever done or lived through and without getting into too many personal details, that speaks volumes. This journey has stripped me bare and it has revealed me to myself on so many levels. It has forced me to make major changes in the way that I live, the company I keep, and the places where I expend my energy. It has forced me to reevaluate my priorities. It has damaged my health and my resilience and it has given me no choice but to examine the various ways I was actively contributing to that damage (because in my case, I absolutely was contributing). The withdrawal process has opened the door for me to find real ways to heal and better ways to live. In this way it has been both the best and the worst thing to ever happen in my life, as odd as that may sound. And today even though my healing is not over, I can truly celebrate having cleared the first hurdle. I am drug free. I am free.
If there is one take away from all of this here it is: we pay the price of time, and there is no way around this truth. The journey off of psychiatric drugs takes time, period. Healing takes time. We can either spend years tapering carefully, or we can spend years trying to recover from tapering too fast. There are no shortcuts. Based on both my own experience and what I have witnessed in many others over the years, I would much prefer the former if given any choice in the matter at all. At least when I finally stabilized on a slow taper I was able to experience moments of joy and meaning and hope, and I was able to do at least some of what is important to me in my life. That sure beats the alternative. Patience is everything on this road, it seems.
Another big takeaway for me: I could not have been successful if I hadn’t been willing to take a good hard look at my life and at myself and do the real work of addressing what was actually fueling my distress and my suffering–because it wasn’t a brain chemical imbalance. For such a long time I believed that there was no good reason for my distress, so there must be something wrong with me. But in reality there was so much that wasn’t working–that had never worked–it just took me a long time to be able to see it for what it was, and an even longer time to have the tools necessary to begin fixing what was wrong. It took me a long time to understand that my dis-ease was actually an invitation to something better for myself. And this is truly my life’s work: honestly looking and asking the hard questions with genuine curiosity and without shame or judgment, so I can do whatever is necessary for me to continue to heal, grow, change, let go, and strip away what doesn’t serve me. And in turn this makes the space for me to replace what I’ve stripped away with things, behaviors, practices, beliefs, surroundings, etc. that do serve me. There has been an unbelievable amount of subtlety in this awakening of my own awareness. For most of my life I didn’t have the tools to do the hard work, and it was a lot less threatening to simply avoid looking too closely, or admitting to myself everything that truly wasn’t working and doing something about it.
But there was just no way I could have completed my taper, and there is no way for me to live a drug free life going forward without that continued honest reckoning with myself. This process of evaluating and re-evaluating myself, my life, and my priorities will be a work in progress for the rest of my days, and that is as it should be. Success for me, in every sense and every situation, means making peace with the process and adapting to what is. In this way we are never “done.” Today I know that even in the deepest depths of suffering–of so-called mental illness–I was never broken. There was never anything wrong with me. I was a human being, having a human experience and that never should have been pathologized by me or by anyone else. And when I finally managed to internalize the truth of my wholeness and my humanity, when it finally took root deep in my being… that’s when, at long last, things began to get easier. It is this knowing that I come back to over and over in times of distress and dis-ease. It is this knowing that illuminates my way forward.
People ask me often if my depression and anxiety symptoms have come back now that I am off my drug. The honest answer is that they never really went away. Not on the drugs, not off them. I still probably meet DSM diagnostic criteria for “persistent depressive disorder” and “generalized anxiety disorder” (albeit meeting the criteria isn’t exactly hard to do). But I no longer identify with any diagnostic labels, and I don’t consider myself depressed or anxious anymore. My understanding of these difficult human experiences that get categorized as depression and anxiety–and their purpose in my life–has changed. So naturally how I interact with them when they show up has changed too. They no longer rule me. They have been integrated as an essential, life-giving part of my own being… because today they serve as guides who alert me to the things that still need my attention, that still need healing, that need to change, and that need love and to be loved. They keep me from going blind and numb to the reality of my own experience. They keep me accountable to that life’s work that will never really be done. Today they are gifts.
I have been incredibly fortunate to have both a therapist (therapist, not psychiatrist) and now a general practitioner who are in my corner. Neither of them understands much about withdrawal but neither of them has ever tried to tell me my experience isn’t real or valid, and both of them have been supportive of my tapering as slowly as I felt I needed to. My therapist told me recently that I have clearly done such a deep dive into the scientific literature and into learning about the realities of SSRI withdrawal that she thinks I could see about finding a university that would help me turn all my hard work into a doctoral degree. My GP, who wrote me my prescription for liquid Celexa during the duration of my taper, said: “I have never had anyone taper anywhere near as slowly as you are but if you have the patience, what’s it to me?” In today’s medical world I think that’s about as good as it gets. It probably also doesn’t hurt that I bring her any relevant scientific literature on the subject that has been published since our last appointment. If I am not advocating for myself, who else will? And I know from experience that when you’re going to tell a doctor something that is outside their scope of belief or understanding you’d better have some evidence to back yourself up if you’re to have any hope of being taken seriously.
And of course I have had the Facebook group, which has saved me. Or maybe more accurately, the group and the people in it have given me the information, tools, support, companionship, and other resources I needed to save myself. I could not have done this alone, and I could not have done this relying solely on the advice of my medical doctors. Today I serve my beloved online community as an admin helping to run the group and my role in that capacity has been such an instrumental part of helping me make some meaning out of all of the suffering and struggle of my tapering and withdrawal process. I honestly don’t know that I would still be alive today without their help and support. I certainly wouldn’t be drug free. The weight of that isn’t lost on me, it humbles me every single day. I will owe everyone in there a debt of gratitude for the rest of my life. And that is the third big take away: don’t try to do it alone, find people who truly understand what you’re going through. There is nothing else like it, and it might just be the thing that saves you.
What comes next for me? Time will tell. Onward and upward, I hope. I’ll continue doing what I can to offer support to those in the thick of the struggle that is psychiatric drug withdrawal. I believe that better things lie ahead for all of us, even when we can’t see it or feel it. The journey may be imperfect and messy and it may look a little different for each one of us but I think there is always a way forward. If anyone reading this is struggling, do whatever you need to do to stay safe and take care of yourself, but don’t lose heart and don’t give up. The rest of our lives are waiting.